Aneurysms: An Overview
By Elise Ewens, OMS III and Bryan Kramer, MD
What is an aneurysm?
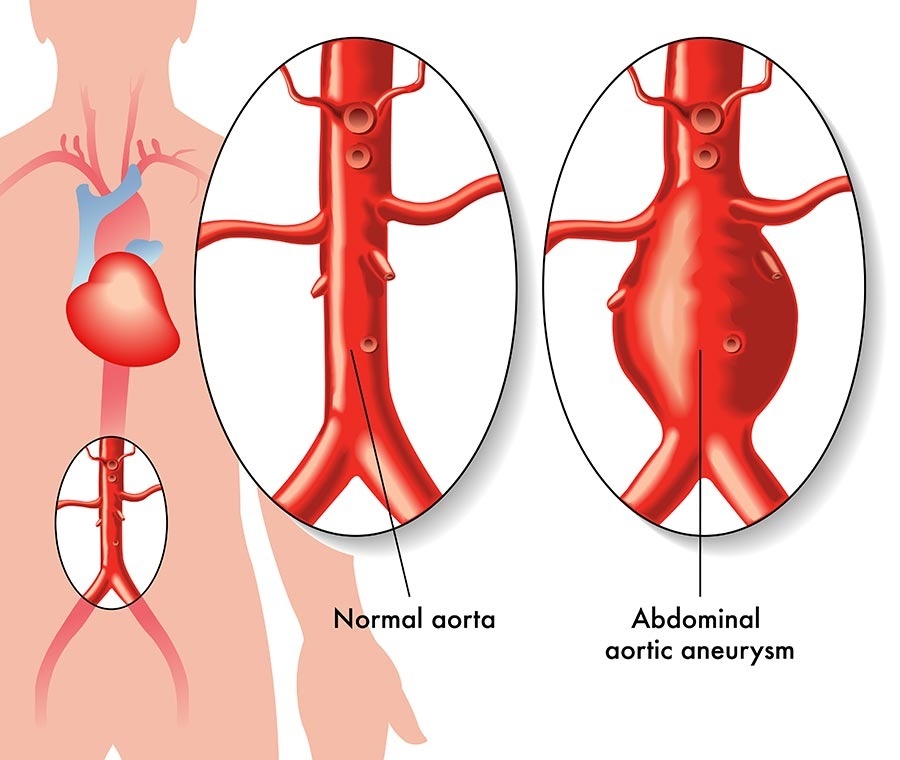
Definition: A weakness in the wall of an artery that causes an abnormal dilation. When most people hear the word “aneurysm” they tend to think of the many complications associated with aneurysms listed below:
While the exact cause of aneurysm formation is not known, any process that weakens or destroys blood vessel integrity can contribute to aneurysm formation. A few risk factors are listed below:
There are many different types of aneurysms depending on the artery affected. Abdominal aortic aneurysms and intracranial saccular aneurysms are two of the most common. Further information on abdominal aortic aneurysms can be found here https://vascularinstitute.com/blog/1161/APatient-s-Guide-to-Abdominal-Aortic-Aneurysm-AAA-. As intracranial aneurysms are within the head, they do not fall under general vascular surgery, but would rather be treated by a neurosurgeon. Peripheral artery aneurysms are a broad category that include aneurysms of most any artery excluding the abdominal and thoracic aorta, coronary arteries or cerebral arteries. An aneurysm of any artery outside the brain is treated by a vascular surgeon.
Treatment Options:
The treatment for aneurysms vary, again, depending on the artery affected. The most common treatment methods for aneurysms are:
Citations:
DynaMed [Internet]. Ipswich (MA): EBSCO Information Services. 1995 - . Record No. T1604421653652, Peripheral Artery Aneurysm; [updated 2020 Nov 30, cited 2020 Dec 12]. Available from https://www-dynamed-com.proxy.rvu.edu/topics/dmp~AN~T1604421653652.
“Aneurysm.” Johns Hopkins Medicine, 2020, www.hopkinsmedicine.org/health/conditions-anddiseases/aneurysm.
Stather PW, Sidloff DA, Rhema IA, et al. “A review of current reporting of abdominal aorticaneurysm mortality and prevalence in the literature.” Eur J Vasc Endovasc Surg 2014; 47:240.
Go Back Definition: A weakness in the wall of an artery that causes an abnormal dilation. When most people hear the word “aneurysm” they tend to think of the many complications associated with aneurysms listed below:
- Rupture
- This would be a surgical emergency. This hemorrhage (excessive escaped blood flow from a vessel) can cause significant hypotension (low blood pressure) and can lead to death if not treated.
- Thrombosis (aka formation of a blood clot)
- When the artery is dilated so much this allows for blood in the aneurysmal area to become slow moving and more prone to forming clots.
- Embolization
- An embolus is a blood clot that has broken off and is now free moving throughout the arterial system. This free blood clot can be transported throughout the arteries until it becomes lodged in a narrowed artery away from its original location. This can result in blockage of blood flow to certain parts of the body. This blockage of blood flow is called ischemia. Symptoms of ischemia due to embolization can cause numerous symptoms dependent on what artery the emboli is in. For example, if an artery supplying one of the limbs is occluded the affected limb can lose sensation, motor function, and become cold, pale, and painful.
While the exact cause of aneurysm formation is not known, any process that weakens or destroys blood vessel integrity can contribute to aneurysm formation. A few risk factors are listed below:
- Smoking
- Hypertension
- Family history
- Advanced age
There are many different types of aneurysms depending on the artery affected. Abdominal aortic aneurysms and intracranial saccular aneurysms are two of the most common. Further information on abdominal aortic aneurysms can be found here https://vascularinstitute.com/blog/1161/APatient-s-Guide-to-Abdominal-Aortic-Aneurysm-AAA-. As intracranial aneurysms are within the head, they do not fall under general vascular surgery, but would rather be treated by a neurosurgeon. Peripheral artery aneurysms are a broad category that include aneurysms of most any artery excluding the abdominal and thoracic aorta, coronary arteries or cerebral arteries. An aneurysm of any artery outside the brain is treated by a vascular surgeon.
Treatment Options:
The treatment for aneurysms vary, again, depending on the artery affected. The most common treatment methods for aneurysms are:
- Conservative management with observation
- In this method, once the aneurysm has been identified there will be regular repeat imaging to monitor the size of the aneurysm. If the aneurysm becomes enlarged to a certain point, then surgical interventions are considered.
- Endovascular repair (minimally invasive)
- Endovascular repair usually requires placement of a stent graft to stabilize the blood vessel at the point of the aneurysm. While this can be done with minimal or no incisions, the downside is that stents require lifetime follow up with imaging, and there is a small chance of needing another procedure to keep the aneurysm fixed. More information on this can be found here https://vascularinstitute.com/blog/5055/A-Patient-s-Guide-to-Endovascular-Aneurysm-Repair-EVAR-.
- Open surgery
- Open surgery is when an incision is made and the involved artery is replaced directly. This is more invasive that a stent, but it is more durable, in that it usually is the only procedure you will need for that aneurysm.
Citations:
DynaMed [Internet]. Ipswich (MA): EBSCO Information Services. 1995 - . Record No. T1604421653652, Peripheral Artery Aneurysm; [updated 2020 Nov 30, cited 2020 Dec 12]. Available from https://www-dynamed-com.proxy.rvu.edu/topics/dmp~AN~T1604421653652.
“Aneurysm.” Johns Hopkins Medicine, 2020, www.hopkinsmedicine.org/health/conditions-anddiseases/aneurysm.
Stather PW, Sidloff DA, Rhema IA, et al. “A review of current reporting of abdominal aorticaneurysm mortality and prevalence in the literature.” Eur J Vasc Endovasc Surg 2014; 47:240.