Colorado Varicose & Spider Vein Treatment
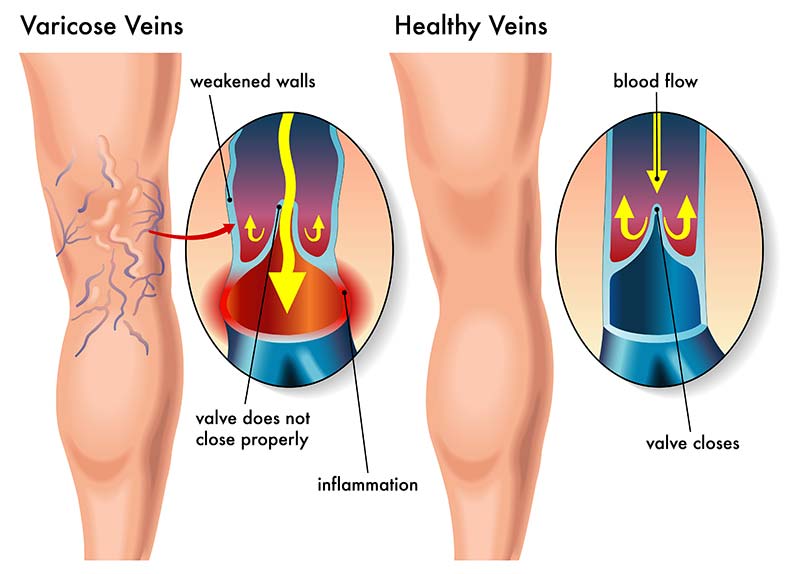
Your legs contain a network of veins which carry the blood back to the heart. Varicose veins are common and present as rope-like blue vessels under the skin, usually a quarter-inch or larger in diameter and are often painful and unsightly. Varicose veins are usually caused by reflux where the vein valves are not working properly causing reversal of blood flow and venous stasis (slow blood flow or pooling). If left untreated, varicose veins may result in leg swelling (Edema), skin changes or in more severe cases, venous ulcers.
Spider veins, or Telangiectasias, are small dilated capillary veins that appear as blue-to-red lines or web-like patterns on legs or around the nose and lips. While they can ache, burn or itch from time to time, they are usually not harmful or symptomatic.
- 20 – 25 million Americans have varicose veins. (American Society for Vascular Surgery)
- 17% of men and 33% of women have varicose veins. (American Society for Vascular Surgery)
Signs and Symptoms
- Heaviness/Fatigue in the legs
- Leg swelling
- Restless Leg Syndrome
- Leg Cramping While Sleeping
- Pain, Itching & Burning
- Blue or red vessels visible under the skin
Risk Factors
- Heredity
- Excess weight or obesity
- Prolonged periods of standing or sitting
- Female
- Pregnancy
- Older Age
Detection
A comprehensive evaluation that includes an ultrasound must be completed to properly detect varicose veins, evaluate blood flow and the efficiency of the vein valves.
Treatment Options
- Varicose Vein Ablation
- This minimally invasive technology provides an alternative to traditional vein stripping surgeries. Using ultrasound guidance, your physician will position the catheter into the diseased vein through a small opening in the skin. The slender catheter delivers radiofrequency (RF) energy to the catheter, which heats the vein wall causing the diseased vein to close so blood is re-routed to other healthy veins. Performed in an outpatient setting, patients who undergo this procedure have good cosmetic outcomes with minimal to no scarring, bruising or swelling and patients can typically resume normal activities within a few days.
- Ambulatory Phlebectomy
- Ambulatory phlebectomy is a method of surgically removing varicose veins. This outpatient procedure uses tiny incisions (stitches are generally not necessary) and scarring and post-operative discomfort is minimal.
- Sclerotherapy
- Sclerotherapy is a cosmetic procedure used to treat varicose and spider veins. A tiny needle is used to inject a solution or sclerosant directly into the vein damaging the lining of the vessel so that it will be adsorbed into the body. Mild discomfort may be felt for one to two minutes during the procedure and multiple sessions may be needed depending in the size and location of the veins. In general, spider veins respond to treatment in 3 to 6 weeks and larger veins in 3 to 4 months.
Call To Schedule An Appointment
303-539-0736
Frequently Asked Questions
Since valves can’t be repaired, the only alternative is to reroute blood flow through healthy veins. Traditionally, this has been done by surgically removing (stripping) the troublesome vein from your leg. The varicose vein ablation procedure provides a less invasive alternative to vein stripping by simply closing the problem vein instead. Once the diseased vein is closed, other healthy veins take over and empty blood from your legs. This varicose vein treatment helps improve leg pain by rerouting blood flow through healthier blood vessels.
During a stripping procedure, the surgeon makes an incision in your groin and ties off the vein, after which a stripper tool is threaded through the saphenous vein and used to pull the vein out of your leg through a second incision just above your calf. In the varicose vein treatment procedure, there is no need for groin surgery. Instead, the vein remains in place and is closed using a special (ClosureFast) catheter inserted through a small puncture. This may eliminate the bruising and pain often associated with vein stripping (i.e., that may result from the tearing of side branch veins while the saphenous vein is pulled out). Vein stripping is usually performed in an operating room, under a general anesthetic, while the varicose vein ablation is performed on an outpatient basis, typically using local or regional anesthesia. Additionally, a vein specialist can provide more personalized patient care during this procedure.
Three randomized trials of the varicose vein ablation procedure vs. vein stripping, including the most recent multicenter comparative trial, show very similar results. In the multicenter comparative trial, the varicose vein ablation procedure was superior to vein stripping in every statistically significant outcome. In the study, 80.5% of patients treated with the varicose vein ablation procedure returned to normal activities within one day, versus 46.9% of patients who underwent vein stripping. Also, varicose vein ablation procedure patients returned to work 7.7 days sooner than surgical patients. Patients treated with the varicose vein ablation procedure had less postoperative pain, less bruising, faster recovery time, and fewer overall adverse events.
The procedure itself usually takes less than 10 minutes, however, one will usually spend 1-2 hours in the procedure room from start to finish depending on adjunctive procedures and pre/post operative preparation and observation.
Patients report feeling little, if any, pain during the varicose vein ablation procedure. Your physician will give you a local or regional anesthetic to numb the treatment area.
The varicose vein ablation procedure can be performed under local, regional, or general anesthesia.
Generally, one may resume normal activities in 1 – 2 days. Many patients can resume normal activities immediately. For a few weeks following the treatment, your doctor may recommend a regular walking regimen and suggest you refrain from very strenuous activities (heavy lifting, for example) or prolonged periods of standing. The recovery time is notably shorter compared to other invasive procedures.
Most patients report a noticeable improvement in their symptoms within 1-2 weeks following the procedure.
Patients report minimal to no scarring, bruising, or swelling following the varicose vein ablation procedure. Superficial veins are treated without significant side effects, minimizing skin discoloration.
As with any medical intervention, potential risks and complications exist with the varicose vein ablation procedure. All patients should consult their vein specialist to determine if their conditions present any special risks. Your physician will review potential complications of the varicose vein ablation procedure at the consultation, and can be reviewed in the safety summary. Potential complications can include: vessel perforation, thrombosis, pulmonary embolism, phlebitis, hematoma, infection, paresthesia (numbness or tingling), and/or skin burn. Blood clots are a possible but rare complication.
Only a physician can tell you if the varicose vein ablation procedure is a viable option for your vein condition. Experience has shown that many patients with superficial venous reflux disease can be treated with the varicose vein ablation procedure. A vein clinic is the ideal place to get a comprehensive evaluation for this procedure.
The most important step in determining whether or not the varicose vein ablation procedure is appropriate for you is a complete ultrasound examination by your physician or qualified clinician. Age alone is not a factor in determining whether or not the varicose vein ablation procedure is appropriate for you. The varicose vein ablation procedure has been used to treat patients across a wide range of ages.
Published data suggests that two years after treatment, 90% of the treated veins remain closed and free from reflux, the underlying cause of varicose veins. This makes it a reliable varicose vein treatment option.
The vein simply becomes fibrous tissue after treatment. Over time, the vein will gradually incorporate into surrounding tissue. One study reported that 89% of treated veins are indistinguishable from other body tissue one year after the varicose vein ablation procedure was performed. Deeper veins continue to function normally, taking over the role of the treated vein.
Many insurance companies are paying for the varicose vein ablation procedure in part or in full. Most insurance companies determine coverage for all treatments, including the varicose vein ablation procedure, based on medical necessity. The varicose vein ablation procedure has positive coverage policies with most major health insurers. Your physician can discuss your insurance coverage further at the time of consultation.
98% of patients who have undergone the varicose vein ablation procedure are willing to recommend it to a friend or family member with similar leg vein problems.
1 - Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O, et al. Prospective randomized study of endovenous radiofrequency obliteration (Closure) versus ligation and stripping in a selected patient population (EVOLVES study). J Vasc Surg 2003;38:207-14.
2 - Goldman, H. Venefit of the greater saphenous vein with endo radiofrequency thermal heating of the vein wall in combination with ambulatory phlebectomy: preliminary 6-month follow-up. Dermatology Surg 2000; 26:452-456.
3 - Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux: a multicenter study. J Vasc Surg 2002;35:1190-6.
4&7 - Weiss RA, et al. Controlled Radiofrequency Endovenous Occlusion Using a Unique Radiofrequency Catheter Under Duplex Guidance to Eliminate Saphenous Varicose Vein Reflux: A 2-Year Follow-up, Dermatologic Surgery, Jan 2002; 28:1: 38-42
5 - Whiteley, MS, Holstock JM, Price BA, Scott MJ, Gallagher TM. Radiofrequency Ablation of Refluxing Great Saphenous Systems, Giacomini Veins, and Incompetent Perforating Veins using varicose vein ablation procedure and TRLOP technique. Abstract from Journal of Endovascular Therapy 2003; 10:I-46.
6 - Pichot O, Sessa C, Chandler JG, Nuta M, Perrin M. Role of duplex imaging in endovenous obliteration for primary venous insufficiency. J. Endovasc Ther 2000;7:451-9.