Signs You Might be Suffering from a Pelvic Venous Disorder
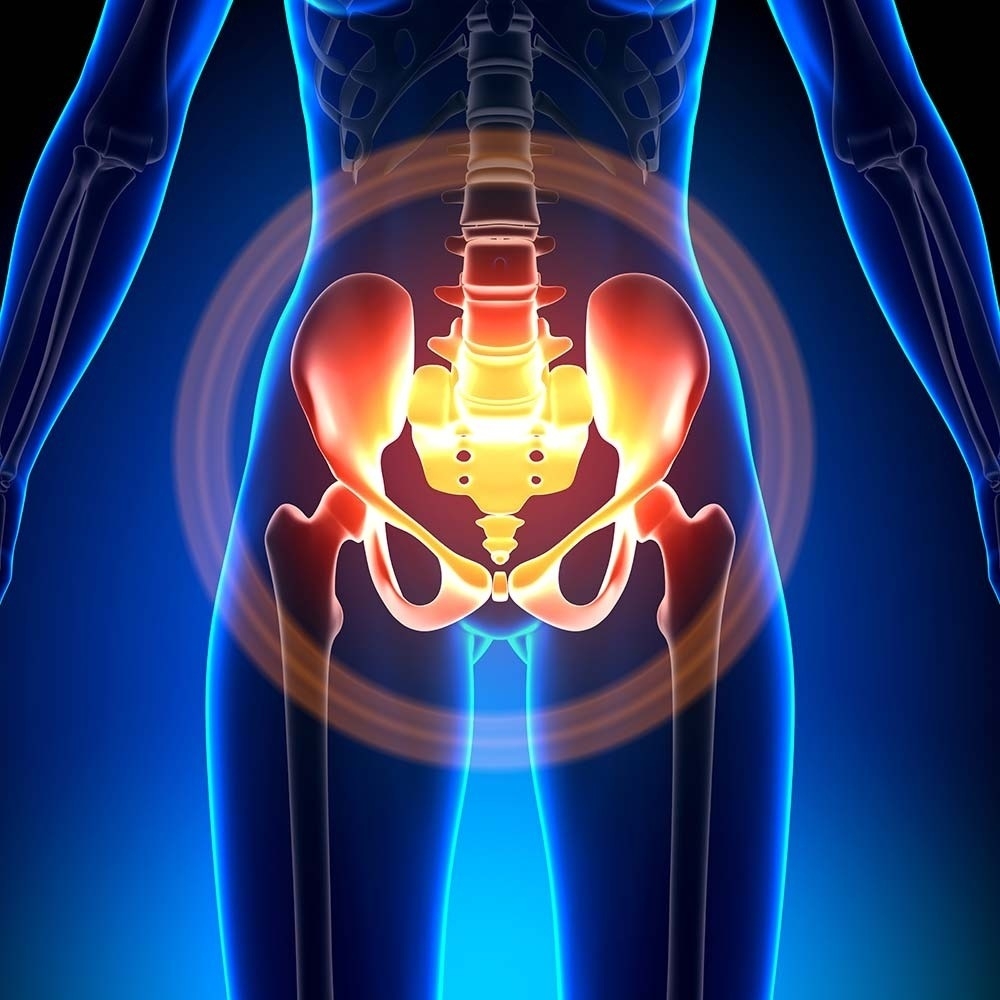
Varicose veins occur as a result of faulty valves which allow blood to fall with gravity and pool in abnormal veins (reflux) or by blockages in the veins not allowing the blood to leave the pelvis (obstruction). Although varicose veins typically occur in lower extremities, such as your lower legs and feet, varicose veins can also occur in your pelvis. Pelvic venous disorders are a painful condition that can occur in both men and women, but it is commonly referred to varicocele in men. Approximately, 13-40% of women that suffer from chronic pelvic pain for more than six months have a pelvic venous disorder.
Signs and symptoms commonly associated with pelvic venous disorders:
Treatment Options
Your gynecologist may start with hormonal medications to reduce the blood flow and engorgement of varicose veins within the pelvis. If the patient does not see improvement, nonsurgical embolization, an outpatient, minimally invasive procedure where a small catheter or plastic tube is inserted into a central vein and guided to the problem veins using X-ray, may be an option. The veins are plugged with foam or coils to prevent abnormal blood flow. Recovery is quick and no stitches are required. Most patients leave the treatment facility/hospital in about four hours and resume normal activities within a few days. Other treatment options include open or laparoscopic surgery to tie the veins. This procedure is more invasive, requires the use of general anesthesia and entails a longer recovery period.
If you are experiencing these symptoms for a period of 6 months or more, please contact your gynecologist today to learn more about a treatment option that works well for you.
To learn more about PVD from Vascular Institute of the Rockies, watch our video here.
Go Back Signs and symptoms commonly associated with pelvic venous disorders:
- Pelvic pain and heaviness
- Pain around the time of menses
- Backache
- Depression
- Fatigue
- Unusual varicose veins around the vulva, buttocks and in between the legs
- Swelling of the labia
- Tenderness of the abdomen
- Burning pelvic pain
- Pelvic floor spasm
- Hip pain
- Feeling of fullness in the legs
- Worsening of stress incontinence
- Worsening irritable bowel syndrome symptoms
- Pain usually affects one side but can affect both
- Pain is worse standing, lifting, during pregnancy or during/after sexual intercourse
- Younger women (<45 years of age)
- Multiple pregnancies (2-3 pregnancies)
- Men with a history of varicocele
Treatment Options
Your gynecologist may start with hormonal medications to reduce the blood flow and engorgement of varicose veins within the pelvis. If the patient does not see improvement, nonsurgical embolization, an outpatient, minimally invasive procedure where a small catheter or plastic tube is inserted into a central vein and guided to the problem veins using X-ray, may be an option. The veins are plugged with foam or coils to prevent abnormal blood flow. Recovery is quick and no stitches are required. Most patients leave the treatment facility/hospital in about four hours and resume normal activities within a few days. Other treatment options include open or laparoscopic surgery to tie the veins. This procedure is more invasive, requires the use of general anesthesia and entails a longer recovery period.
If you are experiencing these symptoms for a period of 6 months or more, please contact your gynecologist today to learn more about a treatment option that works well for you.
To learn more about PVD from Vascular Institute of the Rockies, watch our video here.