Common Causes and Symptoms of Blood Clots
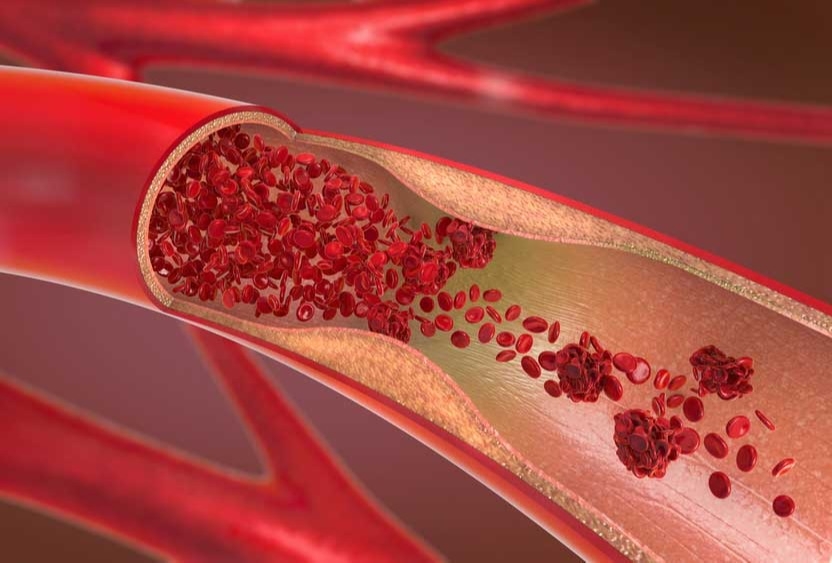
If you are injured and bleeding, your blood will naturally form clots in an effort to stop the bleeding. While the clotting process is critical in this instance, sometimes you can also form clots inside your veins or arteries, which can be dangerous, and even life-threatening. A blood clot that forms in a vein or artery and stays there is called a thrombosis. If part of the clot breaks off and travels elsewhere in your body, such as to the brain or lungs, it is called an embolism.
Other risk factors for blood clots include trauma, some types of major surgery, age, especially over the age of 60, and a family history of blood clots. There are also certain blood disorders and medical conditions that can increase your risk of blood clots.
If you have a clot in your arms or legs, you may experience:
Blood clots are important when it comes to stopping bleeding, but blood clots that form for other reasons can be dangerous. The Vascular Institute of the Rockies has been providing vascular treatments and surgery for over 25 years. Contact us today for treatment and diagnosis of blood clots.
If you have severe chest pain, difficulty breathing, sudden changes in vision or speech, or sudden weakness or numbness of your face or arm, call 911 and seek emergency care right away.
Go Back Common causes
There are several different factors that can cause a blood clot. A clot forms when platelets in your blood start to clump together, which triggers certain proteins, also called clotting factors, to attach to the clot, making it stronger. Other proteins in your blood prevent the clot from becoming bigger than necessary. When a clot is formed in response to an injury, typically your body will begin to break it down as your body heals. However, blood clots can also form if you have poor blood flow. If your blood is allowed to pool in your veins or arteries, the platelets have a higher chance of clumping together and triggering clotting factors and forming a clot. Activities that have a higher risk of clots due to poor blood flow include:- Prolonged sitting: During a long car or plane ride, it is important to try and stretch your legs as much as possible. If you are unable to stand up, you can stretch by doing an exercise movement similar to pumping a gas pedal.
- Prolonged bed rest: During an extended hospital stay, particularly after major surgery or a severe trauma, lack of mobility can cause poor blood flow and allow clots to form. If you are able, you should stretch your calves to promote blood flow.
- Pregnancy: Blood clots during pregnancy can be a result of limited movement, such as bed rest, or poor blood flow to the legs in later pregnancy as the baby presses on blood vessels in the pelvis. Additionally, during pregnancy, in order to minimize blood loss during labor and delivery, your blood clots more easily.
- Birth control pills/hormone replacement therapy/breast cancer medicines: Estrogen, which is often a main component of all three of these types of medicines, can increase clotting factors, while decreasing proteins that stop clotting.
Other risk factors for blood clots include trauma, some types of major surgery, age, especially over the age of 60, and a family history of blood clots. There are also certain blood disorders and medical conditions that can increase your risk of blood clots.
Symptoms
The symptoms you might have are dependent on where the blood clot occurs in the body.If you have a clot in your arms or legs, you may experience:
- Pain or cramping
- Swelling
- Tenderness
- Skin that is red and warm to the touch
- Stomach Pain
- Vomiting
- Diarrhea
- Weakness
- Vision difficulties
Blood clots are important when it comes to stopping bleeding, but blood clots that form for other reasons can be dangerous. The Vascular Institute of the Rockies has been providing vascular treatments and surgery for over 25 years. Contact us today for treatment and diagnosis of blood clots.
If you have severe chest pain, difficulty breathing, sudden changes in vision or speech, or sudden weakness or numbness of your face or arm, call 911 and seek emergency care right away.