Carotid Atherosclerosis
What is Carotid Atherosclerosis?
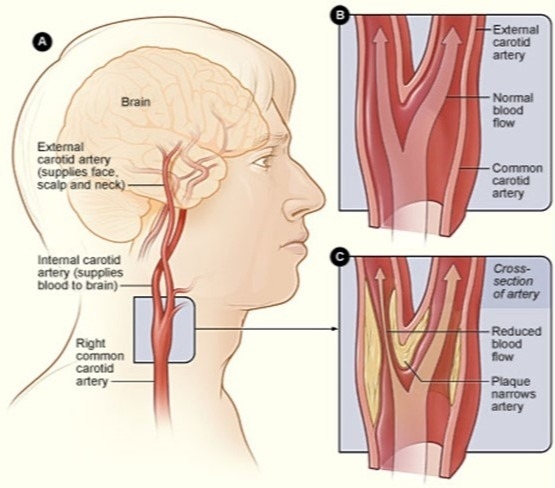
The carotid arteries are a pair of blood vessels located on both sides of your neck that supply oxygenated blood to your brain and head. Over time, buildup of fatty substances and cholesterol create plaques that can narrow the carotid arteries. This reduces the blood flow to your brain and increases the risk of a stroke.
What are the risk factors for Carotid Atherosclerosis?
The major risk factors for carotid atherosclerosis are also the major risk factors for other disease processes that involve blood vessels such as coronary artery disease and peripheral artery disease. These include but are not limited to:
Carotid atherosclerosis may not cause any signs or symptoms until one of the carotid arteries becomes severely narrowed or blocked. The signs and symptoms may include a bruit, a transient ischemic attack (TIA), or a stroke.
As stated earlier, often there may not be presenting symptoms. A TIA or stroke could be the first sign of carotid artery disease. Therefore, it’s crucial to visit your physician regularly for physical exams. They may listen to your carotid arteries to detect a bruit, which could prompt them to obtain an ultrasound of your carotid arteries. An ultrasound is the most common test for diagnosing carotid artery disease. It is a non-invasive test that uses sound waves to create a picture of your carotid arteries, which can detect plaques or narrowing of the vessels. Other diagnostic imaging techniques include carotid angiography, magnetic resonance angiography, and computed tomography angiography.
How is Carotid Atherosclerosis treated?
If you are diagnosed with carotid artery disease, you can meet with one of our vascular surgeons to discuss treatment options and find out what is best for you. The goals of treatment are to stop the disease from getting worse and to prevent strokes. Treatment will depend on how severe the disease and symptoms are, and your overall age and health. Treatments are listed below:
![]()
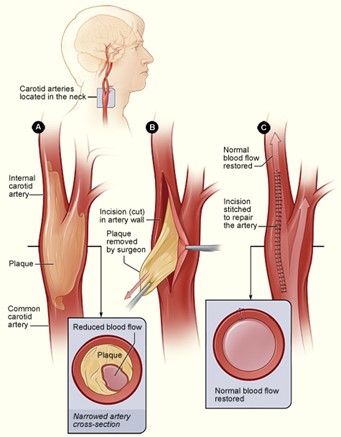
Figure 2: Carotid Angioplasty and Stenting
Sources:
Department of Surgery at UCSF. (2020). Carotid Artery Disease. Retrieved January 16, 2021, from https://surgery.ucsf.edu/conditions--procedures/carotid-artery-disease.aspx
Fairman, R. M. (2020, August 11). Management of symptomatic carotid atherosclerotic disease. Retrieved January 16, 2021, from https://www-uptodate-com.proxy.kcumb.edu/contents/management-of-symptomatic-carotid-atherosclerotic-disease?search=carotid%20artery%20disease%20treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H263202221
Furie, K. L. (2020, June 1). Pathophysiology of symptoms from carotid atherosclerosis. Retrieved January 17, 2021, from https://www-uptodate-com.proxy.kcumb.edu/contents/pathophysiology-of-symptoms-from-carotid-atherosclerosis?search=carotid%20atherosclerosis&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
Go Back The carotid arteries are a pair of blood vessels located on both sides of your neck that supply oxygenated blood to your brain and head. Over time, buildup of fatty substances and cholesterol create plaques that can narrow the carotid arteries. This reduces the blood flow to your brain and increases the risk of a stroke.
What are the risk factors for Carotid Atherosclerosis?
The major risk factors for carotid atherosclerosis are also the major risk factors for other disease processes that involve blood vessels such as coronary artery disease and peripheral artery disease. These include but are not limited to:
- Hypertension – People with high blood pressure are more likely to develop disease in their arteries. The high pressure puts added force against the walls of the artery, which over time makes them more vulnerable to narrowing and plaque buildup.
- Diabetes – Patients with diabetes struggle with high blood sugar levels because their body can’t make enough insulin or doesn’t use its insulin properly. People with diabetes are about four times more likely to have carotid artery disease than those without diabetes.
- Overweight or obesity – Individuals who are overweight typically have higher circulating cholesterol and lipid levels and thus increase their chance for developing atherosclerosis.
- Lack of physical activity – A sedentary lifestyle and lack of exercise can worsen many of the other risk factors for carotid artery disease, such as increased cholesterol levels, high blood pressure, and diabetes.
- Older age – As you age, the risk of atherosclerosis increases. This process of plaque buildup begins as you are younger and progresses over many decades before the disease becomes apparent. Some people may live their entire lives with atherosclerotic disease and never experience any symptoms.
- Smoking – Many chemicals in cigarette smoke cause damage to blood vessels which accelerate the buildup of plaque. Smoking constricts blood vessels and increases blood pressure, while also reducing the amount of oxygen in your blood. This combination increases your risk of a stroke.
- Family history of atherosclerosis
Carotid atherosclerosis may not cause any signs or symptoms until one of the carotid arteries becomes severely narrowed or blocked. The signs and symptoms may include a bruit, a transient ischemic attack (TIA), or a stroke.
- Bruit – A bruit is an audible vascular sound that is associated with turbulent flow through a blood vessel. Your physician may use their stethoscope to listen to your carotid arteries. Sometimes they may hear a blowing sound that could indicate reduced blood flow due to plaque buildup.
- Transient ischemic attack – TIAs are also known as “mini strokes”. The main difference between a stroke and a mini stroke is that a mini stroke may have all or some of the symptoms of a stroke, but the symptoms typically resolve on their own within 24 hours. Signs of a TIA or stroke include:
- Sudden loss of vision, blurred vision, or difficulty in seeing out of one or both of your eyes
- Weakness, tingling, or numbness on one side of your face, one side of the body, or in one arm or leg
- Sudden difficulty in walking or loss of balance
- Sudden dizziness and/or confusion
- Difficulty speaking or swallowing
- Confusion
- Sudden severe headache
- Stroke – Symptoms of a stroke are similar to those of a mini stroke, but can cause lasting brain damage and long term disability. You may have permanent vision or speech problems, paralysis in body parts, and even death.
As stated earlier, often there may not be presenting symptoms. A TIA or stroke could be the first sign of carotid artery disease. Therefore, it’s crucial to visit your physician regularly for physical exams. They may listen to your carotid arteries to detect a bruit, which could prompt them to obtain an ultrasound of your carotid arteries. An ultrasound is the most common test for diagnosing carotid artery disease. It is a non-invasive test that uses sound waves to create a picture of your carotid arteries, which can detect plaques or narrowing of the vessels. Other diagnostic imaging techniques include carotid angiography, magnetic resonance angiography, and computed tomography angiography.
How is Carotid Atherosclerosis treated?
If you are diagnosed with carotid artery disease, you can meet with one of our vascular surgeons to discuss treatment options and find out what is best for you. The goals of treatment are to stop the disease from getting worse and to prevent strokes. Treatment will depend on how severe the disease and symptoms are, and your overall age and health. Treatments are listed below:
- General lifestyle changes – These include maintaining a healthy diet and weight, increasing physical activity, and quitting smoking or drinking alcohol.
- Medications – If stroke symptoms were caused by narrowing of your carotid arteries, many times blood thinners will be used to increase blood flow. Common blood thinning medications include aspirin, warfarin (Coumadin), and clopidogrel (Plavix). Other medications include those that help reduce plaque buildup by decreasing cholesterol levels, such as statins, blood pressure lowering medications like ACE inhibitors, as well as medications that treat diabetes.
- Medical procedures – If symptoms are caused by significant narrowing of your carotid arteries, lifestyle changes and medications may not be enough to treat the disease. Common procedures and illustrations are listed below:
- Carotid Endarterectomy – Typically reserved for symptomatic patients with >50% occlusion or asymptomatic patients with >80% occlusion. Your surgeon will make an incision in your neck and carotid artery and remove the occluding plaque and diseased portions of the artery. This will improve the blood flow to your brain and reduce the risk of future stroke.
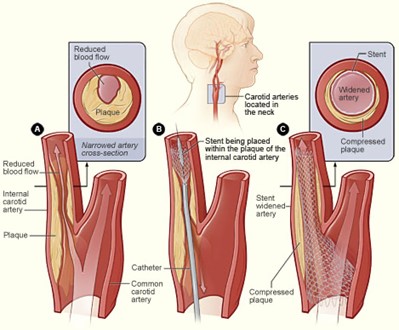
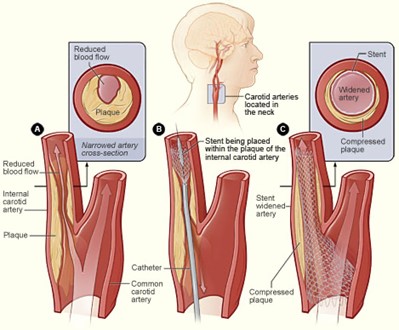
- Carotid Artery Angioplasty and Stenting – This procedure is less invasive than a carotid endarterectomy and involves widening of the arteries to restore blood flow to the brain. The surgeon will guide a thin tube with a deflated balloon into the narrowed portion of the carotid artery. Once positioned correctly, the balloon inflates and pushes the plaque against the wall. A stent is then put in place to reinforce the inner wall of the artery and helps prevent the artery for narrowing in the future.
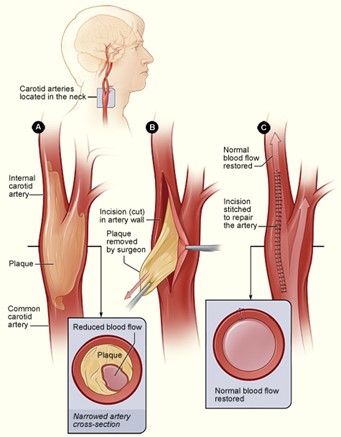
Figure 2: Carotid Angioplasty and Stenting
Sources:
Department of Surgery at UCSF. (2020). Carotid Artery Disease. Retrieved January 16, 2021, from https://surgery.ucsf.edu/conditions--procedures/carotid-artery-disease.aspx
Fairman, R. M. (2020, August 11). Management of symptomatic carotid atherosclerotic disease. Retrieved January 16, 2021, from https://www-uptodate-com.proxy.kcumb.edu/contents/management-of-symptomatic-carotid-atherosclerotic-disease?search=carotid%20artery%20disease%20treatment&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H263202221
Furie, K. L. (2020, June 1). Pathophysiology of symptoms from carotid atherosclerosis. Retrieved January 17, 2021, from https://www-uptodate-com.proxy.kcumb.edu/contents/pathophysiology-of-symptoms-from-carotid-atherosclerosis?search=carotid%20atherosclerosis&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2