Lower Extremity Bypass for Peripheral Artery Disease – Indications and What to Expect
There are several indications for surgical intervention for peripheral artery disease. Some cases may be treated with minimally invasive techniques such as endovascular stenting and angioplasty. Other more complicated cases may require open interventions such as endarterectomy and/or bypass. While bypass surgery is a “real” operation, in many cases it can solve the patients problem for many years or forever, compared to angioplasty and stenting which may need to be repeated frequently to keep the blood flow open.
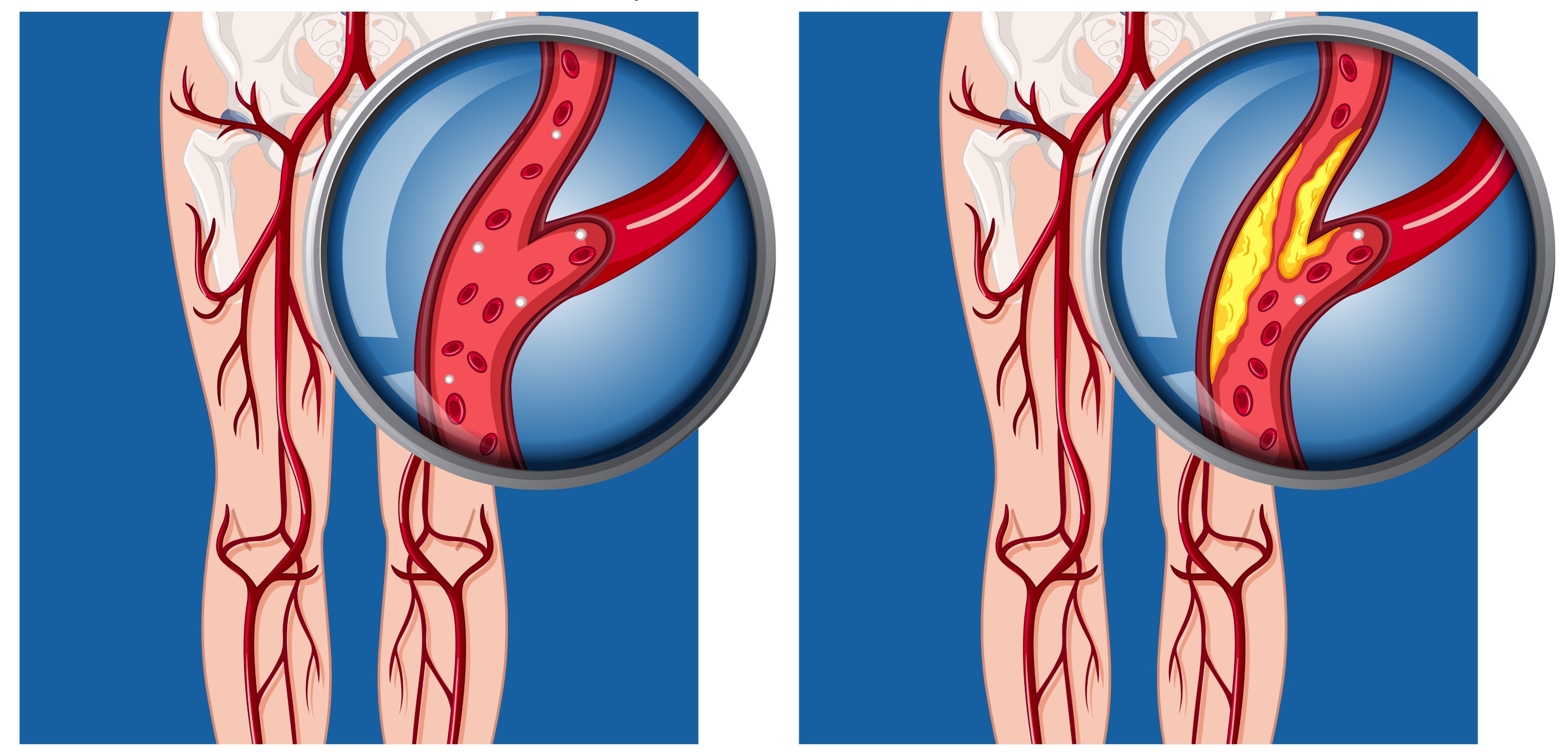
Indications for intervention include pain at rest in the affected limb as well as non-healing wounds from the decreased blood supply. Some may even have a black toe from the lack of blood flow. Patients with peripheral artery disease often have a history of limb claudication, which refers to pain with exertion. For example, when you take a walk down the block, your muscle is consuming oxygen brought to it by the arterial system. When the arteries become narrowed by atherosclerotic plaque, the artery can no longer deliver oxygen to the muscle as it demands. Over time, the patient will complain of pain when walking a certain distance. As the artery narrows more, this can turn into pain at rest at which there is now an indication for surgical intervention. Sometimes we recommend intervention for claudication alone, but not everyone who has a walking limitation needs an intervention. People with claudication alone are not at any risk of limb loss if we do not intervene.
Prior to the peripheral artery bypass procedure, the surgeon will identify a superficial vein from which the bypass graft can be created. Your own veins work best, but sometimes an artificial material such as Dacron or PTFE will be used. Primary patency (the bypass is still open and working) rates at 5 years for saphenous vein grafts are 85.2% vs. PTFE (a prosthetic graft) at 64.5%.1 This is the reasoning for
choosing a native vein as the first choice for grafting material. Typically, the great saphenous vein, that runs along the front and inside of the thigh, is the most common choice. This vein is easily accessed by the surgeon during surgery because its location and path can be easily tracked with ultrasound. Additionally, its location makes it an ideal choice for bypassing some of the large arteries in the leg as they descend down toward the feet. Once the vein of choice has been identified, the surgery team will carefully dissect the vein away from the surrounding superficial tissue. From there, the areas of viable artery will be identified so that the vein graft can be connected to the arterial supply. The goal is to use the vein as a conduit for arterial blood and oxygen delivery to the limb. In order for the vein to act like an artery, we must “arterialize” the vein by removing the venous valves, or take the vein out and reverse its direction of flow. Removing the valves provides a clear path for forward moving blood and further decreases the risk of venous hypertension. Once the vein is arterialized, it can then be placed in its new location with inflow and outflow connections to the artery being bypassed. The flow through the graft is then checked using doppler, which utilizes sound waves to ensure that blood is readily moving through the newly placed graft. Overall, this procedure may seem quite complicated, but a large team of medical experts are involved in the care of each patient. From the ultrasound technologists, to the anesthesiologist, to the surgeons as well as the resident doctors and medical students, there will be a team-based approach to your care.
-Onilia Zorio MS III, Eugenia Jernicks MS III, Garrett Fante MS III
1. Comparisons between prosthetic vascular graft and saphenous vein graft in
femoro-popliteal bypass
Go Back Indications for intervention include pain at rest in the affected limb as well as non-healing wounds from the decreased blood supply. Some may even have a black toe from the lack of blood flow. Patients with peripheral artery disease often have a history of limb claudication, which refers to pain with exertion. For example, when you take a walk down the block, your muscle is consuming oxygen brought to it by the arterial system. When the arteries become narrowed by atherosclerotic plaque, the artery can no longer deliver oxygen to the muscle as it demands. Over time, the patient will complain of pain when walking a certain distance. As the artery narrows more, this can turn into pain at rest at which there is now an indication for surgical intervention. Sometimes we recommend intervention for claudication alone, but not everyone who has a walking limitation needs an intervention. People with claudication alone are not at any risk of limb loss if we do not intervene.
Prior to the peripheral artery bypass procedure, the surgeon will identify a superficial vein from which the bypass graft can be created. Your own veins work best, but sometimes an artificial material such as Dacron or PTFE will be used. Primary patency (the bypass is still open and working) rates at 5 years for saphenous vein grafts are 85.2% vs. PTFE (a prosthetic graft) at 64.5%.1 This is the reasoning for
choosing a native vein as the first choice for grafting material. Typically, the great saphenous vein, that runs along the front and inside of the thigh, is the most common choice. This vein is easily accessed by the surgeon during surgery because its location and path can be easily tracked with ultrasound. Additionally, its location makes it an ideal choice for bypassing some of the large arteries in the leg as they descend down toward the feet. Once the vein of choice has been identified, the surgery team will carefully dissect the vein away from the surrounding superficial tissue. From there, the areas of viable artery will be identified so that the vein graft can be connected to the arterial supply. The goal is to use the vein as a conduit for arterial blood and oxygen delivery to the limb. In order for the vein to act like an artery, we must “arterialize” the vein by removing the venous valves, or take the vein out and reverse its direction of flow. Removing the valves provides a clear path for forward moving blood and further decreases the risk of venous hypertension. Once the vein is arterialized, it can then be placed in its new location with inflow and outflow connections to the artery being bypassed. The flow through the graft is then checked using doppler, which utilizes sound waves to ensure that blood is readily moving through the newly placed graft. Overall, this procedure may seem quite complicated, but a large team of medical experts are involved in the care of each patient. From the ultrasound technologists, to the anesthesiologist, to the surgeons as well as the resident doctors and medical students, there will be a team-based approach to your care.
-Onilia Zorio MS III, Eugenia Jernicks MS III, Garrett Fante MS III
1. Comparisons between prosthetic vascular graft and saphenous vein graft in
femoro-popliteal bypass