May-Thurner Syndrome
What is May-Thurner Syndrome?
May-Thurner Syndrome is an anatomical abnormality in which the Left Iliac Vein is compressed by the Right Iliac Artery.
Why does May-Thurner Syndrome Matter?
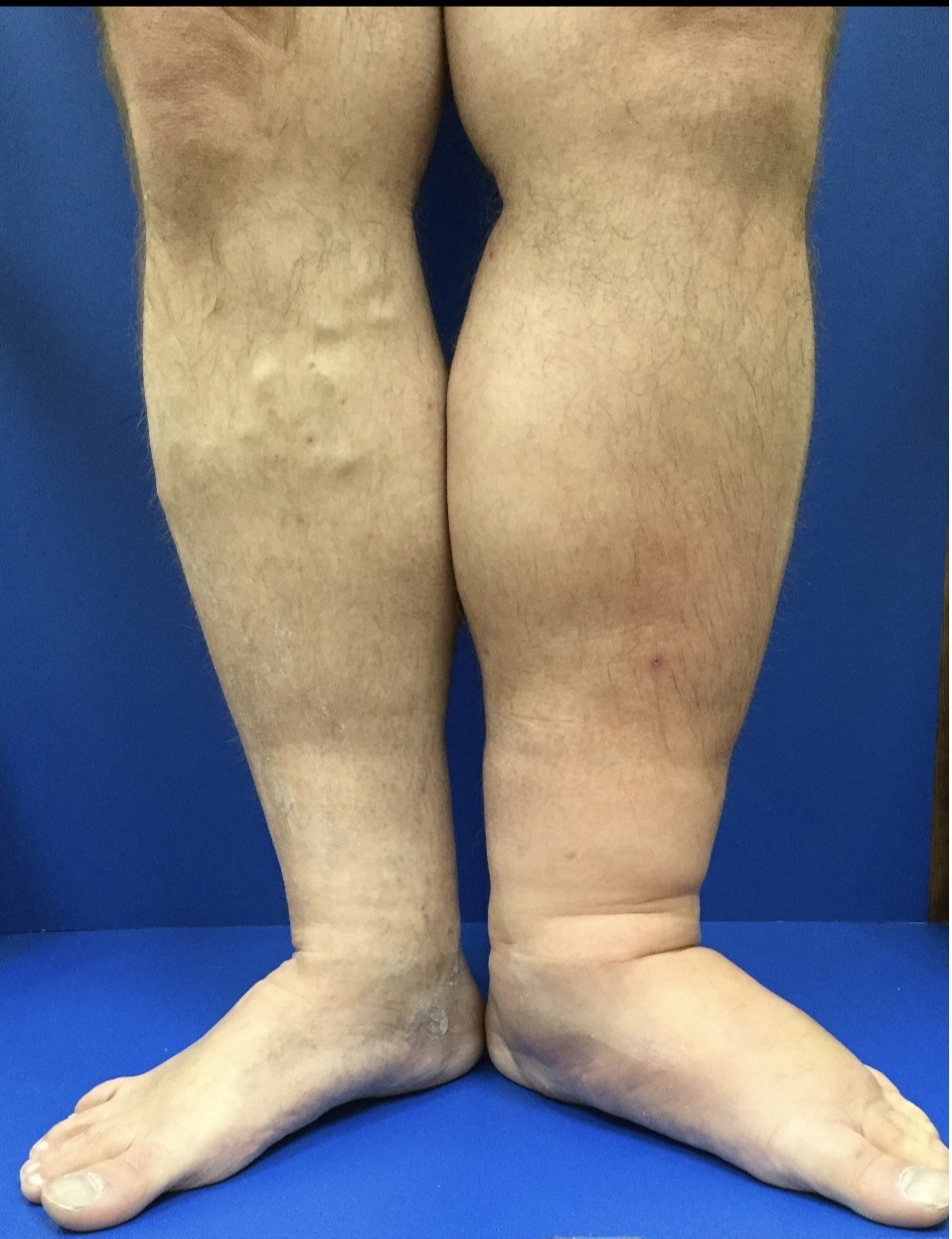
An estimated 3-5% of patients have May-Thurner anatomy. Via Virchow’s Triad, May-Thurner patients are more likely to develop deep venous thromboses (DVTs). In particular, MayThurner patients are at increased risk for massive swelling of the left leg and pulmonary embolism, or even in rare cases Phlegmasia Cerulea Dolens, or “painful blue edema.” The rare patient that develops Phlegmasia has a significantly different prognosis than others with a simple DVT. Their limb may actually be in jeopardy without prompt treatment. Patients who also have a malignancy in addition to May-Thurner are most likely to develop Phlegmasia.
DVT Treatment in May-Thurner Patients
May-Thurner patients are at risk for more problematic DVTs. Similar to patients with typical anatomy, they are started on a heparin drip and the clot is eliminated, often via catheter directed thrombolysis with a TPA infusion. Unlike patients with typical anatomy, May-Thurner patients will require an endovascular stent. Their partially occluded Left Iliac Vein contributed to the formation of a DVT and continues to be at increased risk for DVT. Therefore, they need a stent to ensure that they do not form more DVTs. Lifetime followup is mandatory for any patient with a vascular intervention, like a stent in the iliac vein. We usually do an ultrasound once a year to make sure the vein isn’t narrowing down again. The patient is usually kept on baby aspirin indefinitely as well.
Go Back May-Thurner Syndrome is an anatomical abnormality in which the Left Iliac Vein is compressed by the Right Iliac Artery.
Why does May-Thurner Syndrome Matter?
An estimated 3-5% of patients have May-Thurner anatomy. Via Virchow’s Triad, May-Thurner patients are more likely to develop deep venous thromboses (DVTs). In particular, MayThurner patients are at increased risk for massive swelling of the left leg and pulmonary embolism, or even in rare cases Phlegmasia Cerulea Dolens, or “painful blue edema.” The rare patient that develops Phlegmasia has a significantly different prognosis than others with a simple DVT. Their limb may actually be in jeopardy without prompt treatment. Patients who also have a malignancy in addition to May-Thurner are most likely to develop Phlegmasia.
DVT Treatment in May-Thurner Patients
May-Thurner patients are at risk for more problematic DVTs. Similar to patients with typical anatomy, they are started on a heparin drip and the clot is eliminated, often via catheter directed thrombolysis with a TPA infusion. Unlike patients with typical anatomy, May-Thurner patients will require an endovascular stent. Their partially occluded Left Iliac Vein contributed to the formation of a DVT and continues to be at increased risk for DVT. Therefore, they need a stent to ensure that they do not form more DVTs. Lifetime followup is mandatory for any patient with a vascular intervention, like a stent in the iliac vein. We usually do an ultrasound once a year to make sure the vein isn’t narrowing down again. The patient is usually kept on baby aspirin indefinitely as well.