Peripheral Arterial Disease
By Maria Tran OMS III KCU - February 24, 2020
Peripheral Arterial Disease
By Maria Tran OMS III KCU
Definition
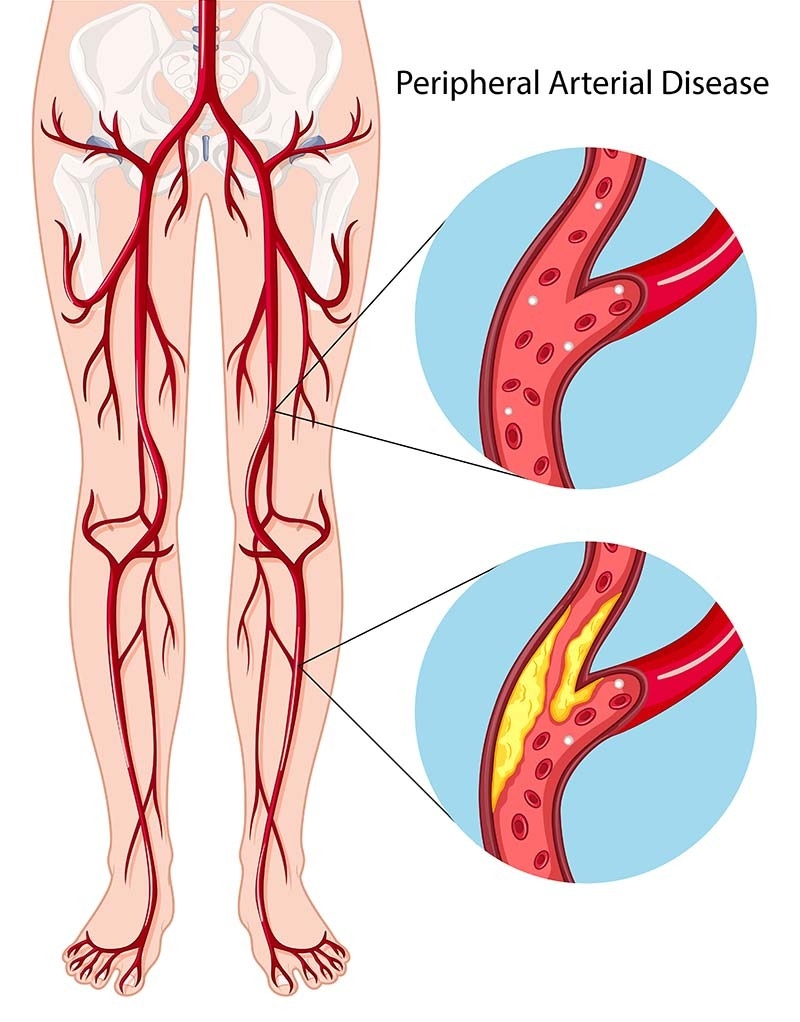
Narrowing and occlusion of the peripheral arteries due to atherosclerosis
Screening and Diagnosis
Clinical diagnosis can be initially made from an array of symptoms including:
- resting pain, cramps, paresthesias distal to arterial occlusion
- Absent or diminished pulses in the brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis arteries
- Decreases in skin temperature, perspiration, hair on legs
- Gangrene, ulcers, necrosis
- Resting pain usually occurs in bed at night and is relieved by dangling the foot off the bed. Dependency improves arterial flow slightly.
- Up to 20-50% of patients with PAD are asymptomatic
- The first-line diagnostic test is an Ankle-brachial Index (ABI) which is highly specific and sensitive
- An ABI is calculated for each leg by dividing the higher systolic pressure of either the dorsalis pedis or posterior tibialis of the respective leg by the higher blood pressure of the right or left arm
- Normal ankle BP and brachial BP are equal to ABI = 1
- Values indicating pathology
- >1.3 = medial sclerosis with an incompressible vascular wall (calcified vessels)
- 1-1.3 = normal value
- 0.91-.99 borderline
- .4-.9 - mild to moderate PAD → Claudication
- <.40 = severe PAD → resting pain, gangrene (critical limb ischemia)
- Exercise testing may be required if a patient has a normal resting ABI. Occasionally we detect diminished flow when muscle demand increases.
- Imaging can help diagnose PAD by locating the site and severity of arterial stenosis or occlusion
- Color-coded duplex ultrasonography
- Digital subtraction angiography (DSA) gold standard
- CT angiography
- MR angiography has largely been replaced by CTA
Asymptomatic Management
● If the patient is not displaying symptoms, treatment is conservative, and consultation is necessary to decrease risk factors.
● Smoking cessation
● Supervised graded exercise therapy
● Foot care (especially in diabetic patients)
● Avoiding cold temperatures
● Medical Therapy to modify cardiovascular risk factors
● Antiplatelet therapy reduces morbidity and mortality
● Aspirin
● ADP receptor inhibitors: Clopidogrel and Ticagrelor
● Lipid-lowering agents (usually Statin)
● Antihypertensive treatment
● Hyperglycemia control
● PDE Inhibitors
● Cilostazol- may improve walking distance with 6 week trial.
Symptomatic Management and Surgical Intervention
● Indications for revascularization procedures include:
● Critical limb ischemia (rest pain, ulcers or gangrene)
● Failure of conservative and pharmacologic treatment
● Claudication is a RELATIVE INDICATION for intervention. About 40% of these patients are disabled on a daily basis and the benefit of intervention outweighs the risk of intervening.
● No co-morbid disease limitations for claudication- if they have COPD, and can only walk a block without getting SOB, fixing their arterial disease is not going to change their life as it will be limited by the COPD
● Vascular surgeons consider minimally invasive endovascular procedures (balloons and stents) FIRST if possible, but open bypass surgery is also an option for some patient. For claudicators, we almost always try medical management first and follow them.
● Vascular surgeons are the only doctors with expertise in all treatment methods for peripheral arteries and veins, and are the only doctors who can perform the best treatment for each individual patient.
● Considerations in choosing treatment include short and long term success of each treatment, risks of the treatment, comorbidities, and patients individual goals for treatment.
Go Back By Maria Tran OMS III KCU
Definition
Narrowing and occlusion of the peripheral arteries due to atherosclerosis
Screening and Diagnosis
Clinical diagnosis can be initially made from an array of symptoms including:
- resting pain, cramps, paresthesias distal to arterial occlusion
- Absent or diminished pulses in the brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis arteries
- Decreases in skin temperature, perspiration, hair on legs
- Gangrene, ulcers, necrosis
- Resting pain usually occurs in bed at night and is relieved by dangling the foot off the bed. Dependency improves arterial flow slightly.
- Up to 20-50% of patients with PAD are asymptomatic
- The first-line diagnostic test is an Ankle-brachial Index (ABI) which is highly specific and sensitive
- An ABI is calculated for each leg by dividing the higher systolic pressure of either the dorsalis pedis or posterior tibialis of the respective leg by the higher blood pressure of the right or left arm
- Normal ankle BP and brachial BP are equal to ABI = 1
- Values indicating pathology
- >1.3 = medial sclerosis with an incompressible vascular wall (calcified vessels)
- 1-1.3 = normal value
- 0.91-.99 borderline
- .4-.9 - mild to moderate PAD → Claudication
- <.40 = severe PAD → resting pain, gangrene (critical limb ischemia)
- Exercise testing may be required if a patient has a normal resting ABI. Occasionally we detect diminished flow when muscle demand increases.
- Imaging can help diagnose PAD by locating the site and severity of arterial stenosis or occlusion
- Color-coded duplex ultrasonography
- Digital subtraction angiography (DSA) gold standard
- CT angiography
- MR angiography has largely been replaced by CTA
Asymptomatic Management
● If the patient is not displaying symptoms, treatment is conservative, and consultation is necessary to decrease risk factors.
● Smoking cessation
● Supervised graded exercise therapy
● Foot care (especially in diabetic patients)
● Avoiding cold temperatures
● Medical Therapy to modify cardiovascular risk factors
● Antiplatelet therapy reduces morbidity and mortality
● Aspirin
● ADP receptor inhibitors: Clopidogrel and Ticagrelor
● Lipid-lowering agents (usually Statin)
● Antihypertensive treatment
● Hyperglycemia control
● PDE Inhibitors
● Cilostazol- may improve walking distance with 6 week trial.
Symptomatic Management and Surgical Intervention
● Indications for revascularization procedures include:
● Critical limb ischemia (rest pain, ulcers or gangrene)
● Failure of conservative and pharmacologic treatment
● Claudication is a RELATIVE INDICATION for intervention. About 40% of these patients are disabled on a daily basis and the benefit of intervention outweighs the risk of intervening.
● No co-morbid disease limitations for claudication- if they have COPD, and can only walk a block without getting SOB, fixing their arterial disease is not going to change their life as it will be limited by the COPD
● Vascular surgeons consider minimally invasive endovascular procedures (balloons and stents) FIRST if possible, but open bypass surgery is also an option for some patient. For claudicators, we almost always try medical management first and follow them.
● Vascular surgeons are the only doctors with expertise in all treatment methods for peripheral arteries and veins, and are the only doctors who can perform the best treatment for each individual patient.
● Considerations in choosing treatment include short and long term success of each treatment, risks of the treatment, comorbidities, and patients individual goals for treatment.