Colorado Peripheral Venous Disease Treatment
PVD develops most commonly as a result of atherosclerosis, or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming a substance called plaque inside the arteries. This is a very serious condition. The clogged arteries cause decreased blood flow to the legs, which can result in pain when walking, and eventually gangrene and amputation. Because atherosclerosis is a systemic disease, individuals with PVD are likely to have blocked arteries in other areas of the body. Thus, those with PVD are at increased risk for heart disease, aortic aneurysms and stroke. PVD is also a marker for diabetes, hypertension and other conditions.
Symptoms
- The most common symptom of PVD is called intermittent claudication, which is painful cramping in the leg or hip that occurs when walking or exercising and typically disappears when the person stops the activity.
- Numbness, tingling and weakness in the lower legs and feet
- Burning or aching pain in feet or toes when resting
- Sore on leg or foot that won’t heal
- Cold legs or feet
- Color change in skin of legs or feet
- Have pain in the legs or feet that awakens you at night
Diagnosis
The most common test for PVD is the ankle-brachial index (ABI), a painless exam in which ultrasound is used to measure the ratio of blood pressure in the feet and arms. The ABI is a simple, painless test that compares the blood pressure reading in the arm and ankle. It is a direct measure of fatty plaque buildup in leg arteries and an indirect gauge of plaque accumulations throughout the entire cardiovascular system.
The blood pressure in your arms and ankles is checked using a regular blood pressure cuff and a special ultrasound stethoscope called a Doppler. The pressure in your foot is compared to the pressure in your arm to determine how well your blood is flowing and whether further tests are needed.
Because atherosclerosis is a systemic disease, individuals developing plaque in their legs are likely to have plaque building up in the carotid arteries, which can lead to stroke, or the coronary arteries, which can lead to heart attack. Early detection of PAD is important because these individuals are at significantly increased risk, and preventive measures can be taken.
- An individual with an ABI of 0.3 (high risk) has a two- to three-fold increased risk of five-year cardiovascular death compared to a patient with an ABI of 0.95 (normal or low risk).
Treatment
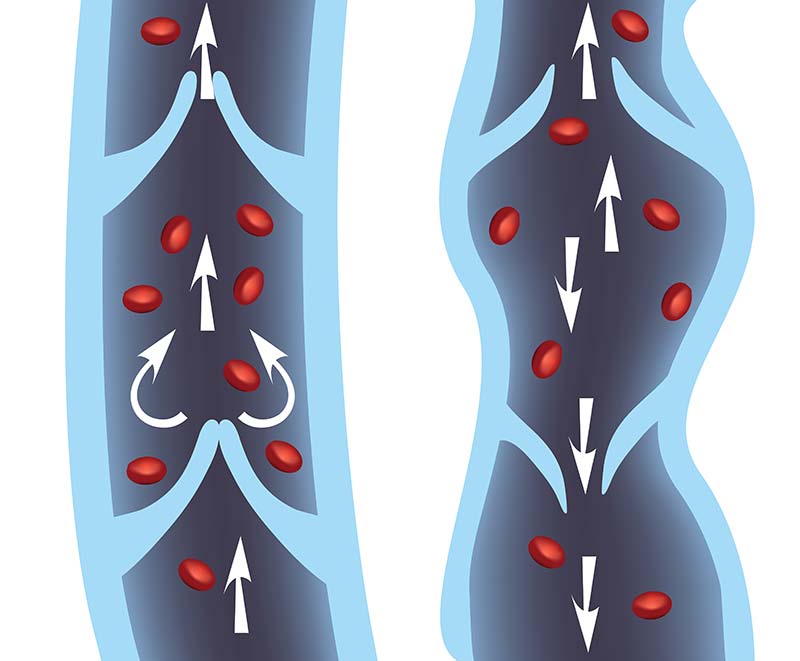
Angioplasty and Stenting
This procedure is considered to be minimally invasive in comparison to open surgery. It is most effective for more localized blockages in the larger arteries. Percutaneous (through the skin) balloon angioplasty, or just "angioplasty," is a technique for enlarging an artery that is blocked or narrowed without surgery. Angioplasty is not a permanent solution for most people. Stenting is a technique for arteries that are very severely blocked or begin to close up again after angioplasty.
- The majority of peripheral vascular lesions can be managed by placement of a stent, a small metal mesh sleeve that is fixed inside the narrowed artery. The stent holds the artery open. Eventually, new tissue grows over the stent. A bare metal stent was the initial approach. However, development of restenosis or fibrous scar tissue growth inside the stent leads to recurrent obstruction.
Endarterectomy
An endarterectomy is a surgical procedure to remove the plaque from your artery. A tiny cutting blade is inserted into the artery to cut the plaque away. This leaves a wide-open artery and restores blood flow through your leg artery. The effectiveness of this method depends upon the particular location and extent of the arterial blockage.
Bypass Surgery
Bypass surgery creates a detour around a narrowed, or blocked, section of a leg artery. This is similar to the artery bypass operation done on the heart. A piece of vein, harvested from another part of your body, or a piece of synthetic artery is used to bypass or detour the obstructed segment of disease, therefore restoring blood flow to the downstream or distal portion of the artery.
Amputation
In extreme cases, especially if your leg has gangrene and is not salvageable, your surgeon may recommend amputating your lower leg or foot. Amputation is a treatment of last resort. Vascular surgeons usually only perform this procedure when the circulation in your leg is severely reduced and cannot be improved by the methods discussed already. More than 90% of patients with gangrene who are seen by vascular specialists can avoid amputation or have it limited to a small portion of the foot or toes.
Call To Schedule An Appointment
303-539-0736